Pode um artigo sobre vitamina D e autoimunidade mudar o modo como se aborda a saúde e a performance?
Após ter escrito o post "Mais um prego no caixão da ausência de evidência do Protocolo Coimbra", fiquei com a sensação de que algo me tinha passado ao lado e não teria prestado atenção à verdadeira importância ou impacto que o artigo de investigação sobre o qual me debrucei poderia ter. Voltei a relê-lo para tentar encontrar o que me tinha escapado.
A conclusão a que cheguei é que este trabalho, focado no uso de altas doses de vitamina D nas doenças autoimunes, pode obrigar a reescrever milhares de artigos científicos, rever como se interpretam análises de sangue e mesmo o modo como se vê (e reduz) o impacto do stress na saúde e na performance.
Não acho que seja exagero, honestamente. Eis 3 razões.
1. Todos os estudos sobre o efeito da vitamina D têm de ser reescritos.
Não é exagero.
Uma das críticas que é feita à vitamina D (muito para lá das críticas directas ao Protocolo Coimbra e ao uso das altas doses no tratamento da autoimunidade) é a aparente falta de eficácia clínica quanto se tentam comprovar as associações demonstradas por estudos epidemiológicos.
Segundo as normas da "medicina baseada na evidência", observar que o tratamento A está relacionado com a melhoria da situação X não permite dizer que A tem um efeito positivo em X. Permite dizer apenas que há uma correlação, e correlação não é o mesmo que causalidade.
Para se concluir pelo efeito de causalidade, são necessários estudos de intervenção. Nesse tipo de investigação, se for demonstrado que o tratamento A melhorou a condição X, então é possível dizer que há um efeito de causalidade entre a intervenção e o outcome.
É aqui que entra a crítica:
Por um lado, existem largas centenas de estudos observacionais epidemiológicos a relacionar baixos níveis de vitamina D e uma série de condições clínicas, desde doenças crónicas, como distúrbios de humor, alterações metabólicas ou doenças oncológicas, até diminuição da performance física e mental.
Por outro, os estudos de intervenção têm falhado em demonstrar a tão desejada causalidade.
É, de facto, difícil encontrar artigos que permitam concluir que a vitamina D tem efeito positivo nessas mesmas condições. (Na verdade, é possível inferir causalidade sem haver estudos de intervenção, usando os critérios de Bradford Hill).
Assim, chegam os autores à conclusão que a vitamina D não tem efeito directo sobre essas condições clínicas, sendo as associações encontradas apenas "coincidências".
É exactamente isto que agora muda, após a publicação do artigo Vitamin D Resistance as a Possible Cause of Autoimmune Diseases: A Hypothesis Confirmed by a Therapeutic High-Dose Vitamin D Protocol
Baseando-se nos estudos VitDMed e VitDBol, que mostram existir uma percentagem significativa de pessoas consideradas "low responders" à vitamina D, Lemke et al. dizem-nos que a mesma quantidade de vitamina D pode ter impacto real diferente em pessoas diferentes e que o aumento das concentrações sanguíneas não é um método fiável para avaliar qual o impacto da toma desta hormona.
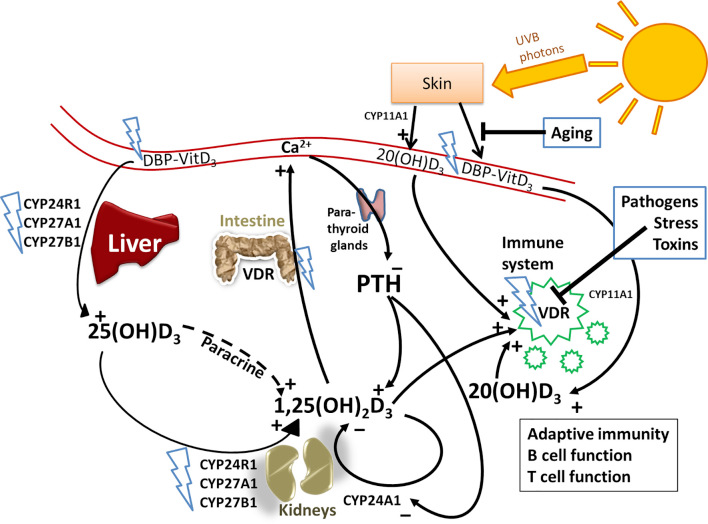
Descrevem também qual será o mecanismo mais fiável para o fazer: a variação da hormona paratiroidea (PTH), tal como fazemos no Protocolo Coimbra. Esta hormona constitui um mecanismo de feedback directo do metabolismo da vitamina D, estando altamente associada às mudanças dos efeito fisiológico efectivo desta vitamina (e não apenas da sua concentração sanguínea).
Imagem retirada de https://pubmed.ncbi.nlm.nih.gov/33897704/
Quando investigadores pretendem avaliar se a toma de vitamina D pode melhorar a doença X, construem um protocolo de investigação no qual constituem dois grupos de pessoas iguais - um grupo toma uma quantidade A de vitamina D e o outro grupo não - comparando depois os dois grupos em relação à actividade ou gravidade da doença, partindo do princípio de que a mesma quantidade de vitamina D e o mesmo aumento da sua concentração sanguínea terá sempre o mesmo efeito, mesmo em pessoas diferentes.
Agora sabe-se que estes protocolos de investigação estão fundamentalmente incorrectos: a mesma quantidade e o mesmo aumento da sua concentração tem efeitos clínicos diferentes em pessoas diferentes.
O efeito fisiológico da vitamina D é atingido quando a PTH está no terço inferior do intervalo de referência, independentemente da sua concentração sanguínea.
"Por outras palavras, se os níveis de 25(OH)D3 estão altos, a PTH deverá estar baixa e vice-versa" (Lemke, et al.)
Dita então a lógica que
Se a PTH não está entre 15 e 31,6ng/mL (considerando o intervalo de referência de 15-65ng/mL), então a vitamina D não estará a ter impacto fisiológico real;
Se não estará a ter impacto real, não se pode saber realmente se a vitamina D não teve impacto porque realmente não tem qualquer efeito nessa condições ou apenas porque ainda não existe em quantidade suficiente para fazer efeito;
Se não se pode isolar o efeito real da vitamina D, não se podem tirar conclusões, seja positivas ou negativas.
Por essa razão, todos os estudos que usem a mesma dose de vitamina D em todos os participantes, sem verificarem a PTH, não podem concluir pela existência ou ausência de efeito da vitamina D.
Mergulhemos então em algumas meta-análises (trabalhos que avaliam as conclusões de artigos publicados, organizando-os de forma rigorosa e sistematizada) para avaliar qual a quantidade de estudos que tiveram esta relação em consideração ou, em sinal oposto, terão de ser redigidas.
Cochrane, 2014, reviu a evidência do impacto da vitamina D nos níveis de mortalidade. Dos 159 estudos incluídos, apenas um estudou a variação da PTH (sem considerá-la um marcador de eficácia). Apesar terem concluído que a vitamina D3 poderia reduzir a mortalidade por todas as causas, em particular por cancro, os estudos e as suas conclusões têm de ser revistos por não terem usado a PTH marcador, não avaliando o efeito real da vitamina D.
British Medical Journal, 2019, novamente sobre o impacto da vitamina D na mortalidade, desta vez incluíram 50 artigos. Nem uma palavra sobre a PTH. Apesar de também concluírem uma redução de 15% da mortalidade, os estudos e as suas conclusões têm de ser revistos por não terem usado a PTH marcador, não avaliando o efeito real da vitamina D.
Nutrients, 2018, sobre o impacto da vitamina D no controlo glicémico na diabetes tipo 2. Foram avaliados 20 estudos diferentes. Apesar de terem encontrado resultados positivos na redução da resistência à insulina, os estudos e as suas conclusões têm de ser revistos por não terem usado a PTH marcador, não avaliando o efeito real da vitamina D.
Nutrients, 2015, sobre o impacto da vitamina D na síndrome do ovário poliquístico. Foram incluídos 30 estudos. Não encontraram efeito positivo mas os estudos e as suas conclusões têm de ser revistos por não terem usado a PTH marcador, não avaliando o efeito real da vitamina D.
PLoS One, 2019, sobre o impacto da vitamina D na força muscular, onde estudaram 8 artigos. Apesar de terem encontrado resultados positivos em alguns grupos musculares, os estudos e as suas conclusões têm de ser revistos por não terem usado a PTH marcador, não avaliando o efeito real da vitamina D.
Sports Medicine, 2017, sobre o impacto da vitamina D na performance desportiva em atletas, tendo incluído 13 estudos. Não encontraram efeito positivo mas os estudos e as suas conclusões têm de ser revistos por não terem usado a PTH marcador, não avaliando o efeito real da vitamina D.
Repare, não estou a querer dizer que a vitamina D teria efeito positivo nos estudos que o não mostraram ou que teria um efeito mais positivo nos que encontraram esse mesmo efeito.
Independentemente de terem obtido resultados positivos ou não, todos os artigos que não incluíram a variação da PTH no seu protocolo de investigação têm de ser reescritos e têm de ter em consideração o impacto individual que a vitamina D tem.
Caso contrário, os estudos não são clinicamente úteis e as suas conclusões falsas.
Seria o mesmo de dizer "beber água, nesta quantidade que não sabemos se é suficiente, não é capaz de melhorar a sede". Ou "inalar menos oxigénio do que o necessário para ter efeito não é capaz de melhorar a falta de ar". É óbvio que uma intervenção insuficiente não vai ter efeito suficiente!!!
2. Valores sanguíneos "normais" não significam que haja um efeito normal
O raciocínio base dos investigadores é simples e lógico: ter uma quantidade "normal" de um composto em circulação só corresponde a um efeito adequado se o sistema estiver a funcionar de forma ótima. Não basta só medir a sua concentração em circulação, é necessário avaliar o seu resultado prático fisiológico e clínico.
Não é este o mesmo tipo de raciocínio que é usado em diferentes cenários para avaliar a eficácia de um sistema?
O sucesso de uma fábrica de mesas depende de quantas mesas consegue produzir por dia já que é esse o real factor que vai determinar a sua viabilidade financeira. A sua rentabilidade dependerá da eficiência com que consegue transformar a madeira que entra na fábrica em mesas para por no mercado.
Na fábrica ideal, a eficiência é sempre 100%: todas as máquinas estão perfeitamente afinadas, funcionam sem qualquer falha, conseguem produzir mesas sem qualquer desperdício de material. Por funcionar de um modo tão eficiente, o número de cadeiras produzido será igual à quantidade de madeira que entra na linha de produção. Por isso, basta manter um abastecimento adequado constante de matéria prima para garantir o sucesso.
Na fábrica real o cenário é diferente.
Nem todas as máquinas funcionam bem, a sua produção é influenciada por diferentes factores - ambientais, estruturais, humanos - e a sua eficiência não é perfeita.
Isto significa que, mesmo usando a exactamente a mesma matéria prima da fábrica ideal - a mesma madeira, na mesma quantidade - o outcome será diferente: o número de mesas produzidas será certamente menor, comprometendo a viabilidade da empresa.
A quantidade adequada de "matéria prima a entrar na linha de produção" deixou de ser a única métrica necessária controlar porque deixou de conseguir prever com rigor a quantidade de mesas produzidas. Não basta saber a quantidade de madeira que entra, é obrigatório medir a quantidade de mesas que sai: é a única forma de avaliar a sustentabilidade e viabilidade da fábrica.
Se substituirmos "madeira" por "vitamina D" e "mesas" por "PTH", chegamos ao raciocínio de Dr Lemke.
Mas podemos não ficar por aí, já que há uma mensagem nas entrelinhas que obriga a parar e pensar:
"valores analíticos sanguíneos normais ou adequados não se traduzem automaticamente num efeito ou equilíbrio ideal".
Há muitas situações semelhantes à da Vitamina D / PTH, nas quais olhar para um produto em circulação não prediz automaticamente o seu impacto real:
Valores sanguíneos ideais de vitamina B9 e B12 podem não ser suficientes se o valor de homocisteína não estiver ideal
Glicémia dentro de valores de referência pode não significar que está tudo bem se a insulina estiver mais alta do que deveria
Sem o valor de DHEA-s, o aumento matinal do cortisol adequado não permite garantir que o ritmo circadiano está mantido
Concentrações "normais" de vitamina C não significam produção suficiente de glutationa celular (ou cortisol)
São alguns exemplos nos quais avaliar só um lado da equação não nos dá a visão abrangente necessária para saber com maior exactidão como o organismo está a funcionar, identificar sinais subtis de alteração fisiológica ou implementar estratégias precoces de melhoria e otimização da saúde e performance.
São a diferença entre ser "normal" ou estar à frente da norma, ou entre não estar doente e ser saudável. Parece o mesmo mas não é.
3. Como o stress tem impacto na saúde e performance humana
Esta parte não está escondida nas entrelinhas do artigo mas é a cola que une peças diferentes, dando mais uma explicação ao impacto do stress no organismo
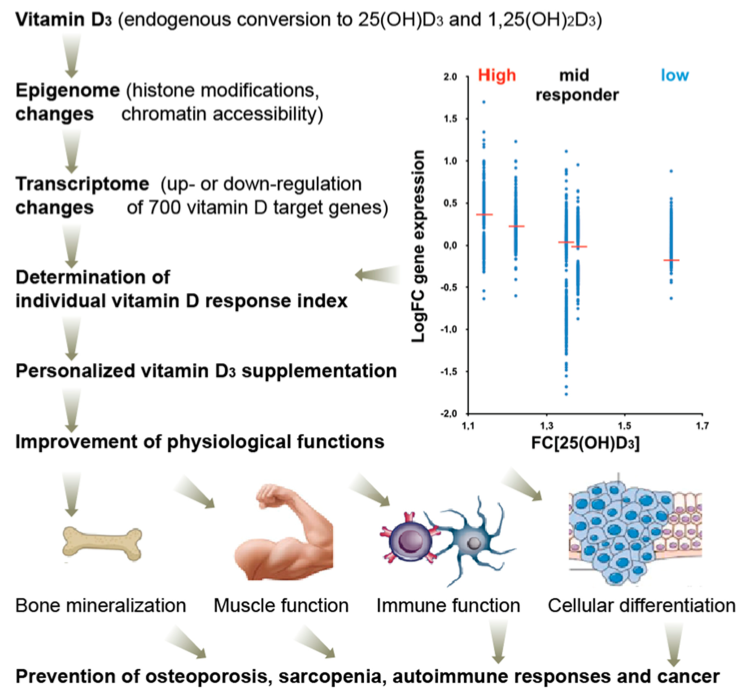
A equipa do Dr Lemke foi bastante clara ao descrever o modo como o stress, em particular emocional, influencia a eficácia da vitamina D ao reduzir a expressão do receptor da vitamina D, o VDR.
O aumento do nível de cortisol, acontecimento típico de quando há mais stress, inibe o VDR e, com isso, reduz o efeito da vitamina, resultando no que os autores chamam de resistência adquirida à vitamina D.
Esta relação explica porque a vastíssima maioria dos nossos doenças que iniciam o Protocolo Coimbra reportam uma associação clara em eventos stressantes ou aumentos dos níveis de stress e agravamento clínico da sua doença.
Explica também porque a maioria dos doentes que infelizmente não sente melhorias com o tratamento apresentam níveis muito altos de stress crónico, em particular emocional.
Conclusão: aumento dos níveis de cortisol diminuem a eficácia biológica da vitamina D.
O problema é que este efeito não está limitado à autoimunidade!
Imagem retirada de https://www.mdpi.com/2072-6643/11/3/676/htm
Em situações em que existem níveis cronicamente elevados de cortisol, há uma redução de todos os efeitos da vitamina D. Isto acontece porque ela exerce o seu efeito ligando-se ao VDR e, em conjunto, influenciam a transcrição genética de mais de 1000 genes .
O impacto é particularmente significativo em 3 sistemas:
Neurológico
Imunitário
Osteomuscular
Uma melhor saúde e performance obriga à otimização destes sistemas. Em qualquer que seja o contexto - seja um corporate athlete , weekend warrior, um atleta profissional ou querer ser saudável para viver melhor - temos todos de concordar que as funções cerebral, imunitária e muscular são peças fundamentais para o sucesso!
Sem conseguir pensar ou tomar decisões, defender e recuperar ou ter força e resistência estrutural, atingir os objectivos ficará muito mais difícil.
Acontece que a vitamina D influencia muito o modo como estes sistemas actuam!
"Baixos níveis de vitamina D predizem disfunção executiva, em particular mental shifting, actualização da informação e velocidade de processamento". (artigo)
"A função adequada do sistema de defesa do nosso corpo requer a presença de níveis adequados de vitamina D para a integridade da barreira, produção de compostos antimicrobianos, quimiotaxia de outras células imunitárias e regulação os sistemas imunes inato e adaptativo" (artigo)
"Status pobre de vitamina D afecta força muscular e a vitamina D poderá participar na síntese proteíca através das acções do VDR no tecido muscular. Poderá também proteger contra lesões de sobre-uso, como as fracturas de stress, através do seu papel no metabolismo do cálcio". (artigo)
Logo, se os níveis altos de cortisol reduzem a eficácia da vitamina D, irão também reduzir a função cognitiva, a eficácia imunitária e a performance desportiva!
O trabalho de Lemke et al., ajuda a esclarecer o modo como stress diminui a nossa saúde e reduz a nossa performance. É a cola que ajuda a unir estas peças.
Mas levanta também uma hipótese de como reduzir este impacto. Se:
Uma das razões para o processo autoimune é o impacto dos níveis altos de cortisol resultantes de stress
Usando doses mais altas de vitamina D conseguimos melhorar a sua função ao ponto de ser possível reduzir ou desligar uma doença autoimune, conseguindo reverter o efeito do cortisol
O efeito adequado de vitamina D é atingido quando a PTH está baixa
Então é justo pensar que o uso de vitamina D em doses eficazes personalizadas pode conseguir diminuir o impacto negativo do stress, contribuindo para uma melhoria da saúde e da performance!
O que me leva a uma questão: