Como intolerâncias alimentares podem ser parte de um título mundial
A área da medicina que mais me apaixona é a optimização da performance humana, procurar e adoptar estratégias para superar os limites, estar à frente da competição e atingir o topo. Fascina-me a endurance e os atletas que são capazes de ultrapassar várias vezes os limites do ser humano, em particular os que conseguem nadar 3,8km em águas abertas, percorrer 180km de bicicleta e terminar correndo uma maratona.
Se já acharia incrível conseguirem esse feito num dia, como apelidar quem o consegue fazer em 8h?!
Lucy Charles-Barclay (fonte: Instagram @lucycharles93)
Uma dessas atletas que sigo nas redes sociais é a Lucy Charles-Barclay, antiga nadadora britânica tornada triatleta, que se congragou há poucos dias campeã mundial de Ironman 70.3, após ter ficado várias vezes em segundo lugar. Num vídeo do seu canal de Youtube, partilhou ter feito recentemente um teste de intolerâncias alimentares. Não sendo necessariamente surpreendentes, os resultados obrigariam a uma alteração significativa do seu plano alimentar.
O objectivo, segundo Lucy diz, seria tentar ganhar 1 a 2% de performance.
Quando se compete ao mais alto nível, qualquer ganho de performance não pode ser menosprezado. Apesar de parecer um valor pequeno, ganhar 1 ou 2% em 8 horas de prova pode representar um ganho real de 5 a 10 minutos o que é a diferença entre vencer ou não vencer (nos campeonatos mundiais de Ironman 2019, em Kona, Hawai, a diferença entre o primeiro e quarto classificados na prova masculina foi de pouco mais de 11 minutos).
Não tenho qualquer espécie de inside knowledge que me permita saber qual o impacto real desta alteração e a relação que teve com o título mundial. Resta-me mergulhar na ciência e tentar chegar a alguma conclusão. Foi exactamente isso que tentei fazer.
Porque surgem as intolerâncias alimentares
Uma intolerância alimentar surge quando o organismo reage contra parte de um alimento, desencadeando uma reacção imunitária de maior ou menor magnitude, com maior ou menor impacto clínico.
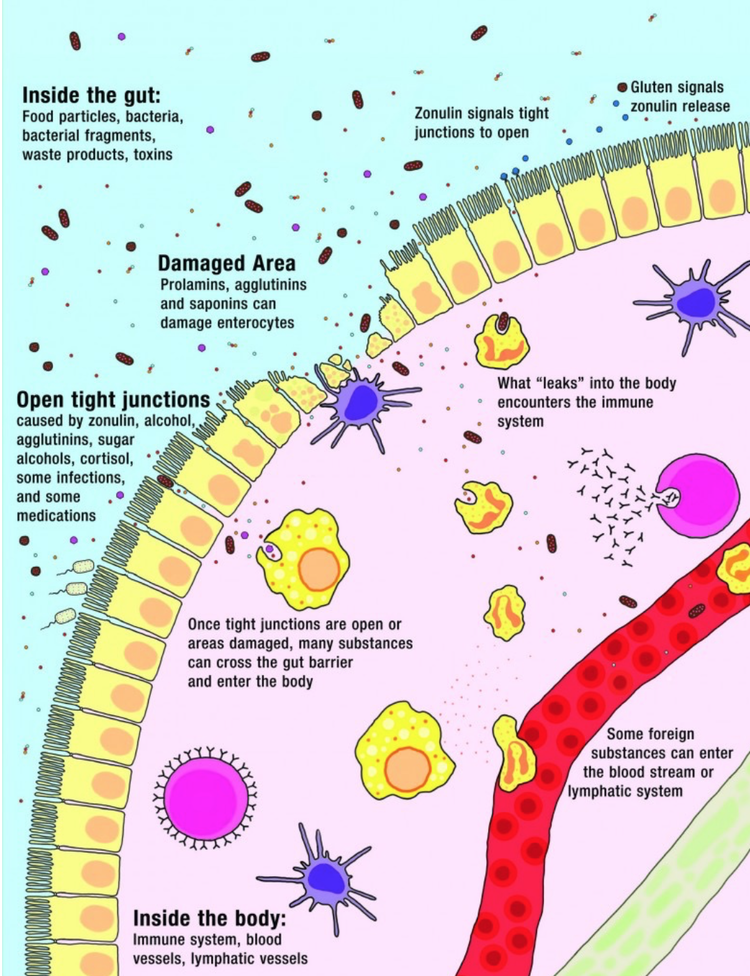
Quando tudo está bem, ingerimos um alimento e somos capazes de o digerir. O processo digestivo decorre normalmente e somos capazes de o dividir em partes progressivamente mais simples para que possam ser absorvidos no intestino, no local certo, pelo canal ou receptor certo, entrando assim realmente no nosso organismo.
Após a passagem pela a mucosa intestinal (a barreira física de células), os componentes absorvidos são analisados pelo sistema imunitário residente, o GALT - gut-associated lymphoid tissue, que scaneia tudo o que acabou de entrar, assegurando-se que não encontra qualquer inimigo ou razão para alarme.
Quando assim é, deixa entrar livremente no nosso sistema, para que possa ser usado pelas nossas células.
Este processo ocorre sempre que comemos ou bebemos. É de tal forma importante para a nossa saúde que a maior parte das nossas células imunitárias estão localizadas no intestino de modo a garantir que conseguimos discernir amigos de inimigos.
É assim que nos mantemos seguros.
No entanto, quando este processo não ocorre desta forma e o sistema imunitário identifica alguns dos compostos como perigosos ou inimigos, desencadeamos uma reacção de defesa contra esses "agressores". Deixamos de ser tolerantes a esses alimentos, havendo várias razões para isto acontecer. Qualquer que seja a razão, a reacção que causam é a mesma:
o aumento da libertação de mediadores pró-inflamatórios, como a IL6 ou TNFa;
o aumento da mobilização e activação de células imunitárias, como os neutrófilos e macrófagos M1
a criação de um estado inflamatório local com possibilidade de se tornar num quadro sistémico.
Estes desequilíbrios devem merecer a atenção de quem procura atingir o seu melhor nível de performance, desde os melhores do mundo como a Lucy, a weekend warriors que procuram superar-se, a quem se preocupa em manter a saúde ou mesmo os corporate athletes.
Que impacto têm?
O impacto das intolerâncias alimentares na performance física e mental deve-se à influência que exercem no processo que está no centro da recuperação do esforço físico e de adaptação ao treino: inflamação.
Os atletas treinam para evoluírem, se tornarem mais fortes e resistirem melhor à fadiga. Tentam que cada sessão de treino resulte em mais um passo em direcção ao seu objectivo. Para isso acontecer, tem de resultar em alterações e adaptações bioquímicas e fisiológicas que, cumulativamente, originarão um ganho de performance.
Esta lógica está subjacente a todos os tipos de treino. Usando a corrida como exemplo, treinos longos abaixo da frequência cardíaca MAF melhoram a eficiência cardiovascular e da função mitocondrial enquanto que sprints resultam num aumento da densidade mitocondrial e rapidez das fibras musculares. Ambos estimulam algum nível de adaptação das células musculares e estruturas de suporte, como osso, tendões e ligamentos, que, em conjunto, resultaram em melhores tempos de corrida.
Apesar de serem treinos extremamente diferentes - as fibras musculares recrutadas, os sistemas de produção de energia e até o esforço mental são diferentes -, os ganhos só existem se o sistema der um passo em frente rumo à melhoria da performance.
Essa caminhada faz-se de ciclos contínuos de destruição e reconstrução, desencadeados por cada treino, por cada estímulo. O sucesso desse processo depende da orquestração perfeita das duas fases do ciclo, tanto em magnitude como em timing: se a destruição é demasiado grande, a reconstrução vai ser mais difícil e demorada; se a reconstrução é lenta, o novo estado não vai ser melhor ou mais forte.
Qual a força controladora deste processo de evolução, ganho e progressão? Inflamação.
Longe vai o tempo em que a inflamação era vista apenas como uma força maléfica que destruía e eliminava qualquer ganho resultante do treino. Não era uma visão descabida ou desprovida de sentido: há dados a suportar este efeito destrutivo, em particular o efeito catabólico que resulta de quadros inflamatórios crónicos sistémicos. Aliás, este é um ponto importante em termos de performance, a que iremos voltar.
A inflamação controla todo o ciclo de adaptação ao treino. O segredo está na orquestração perfeita entre as duas fases, no equilíbrio entre a pró-inflamação, que desencadeia a destruição, e a anti-inflamação, que acciona a recuperação. Deixe-me usar o músculo como exemplo de como tudo ocorre.
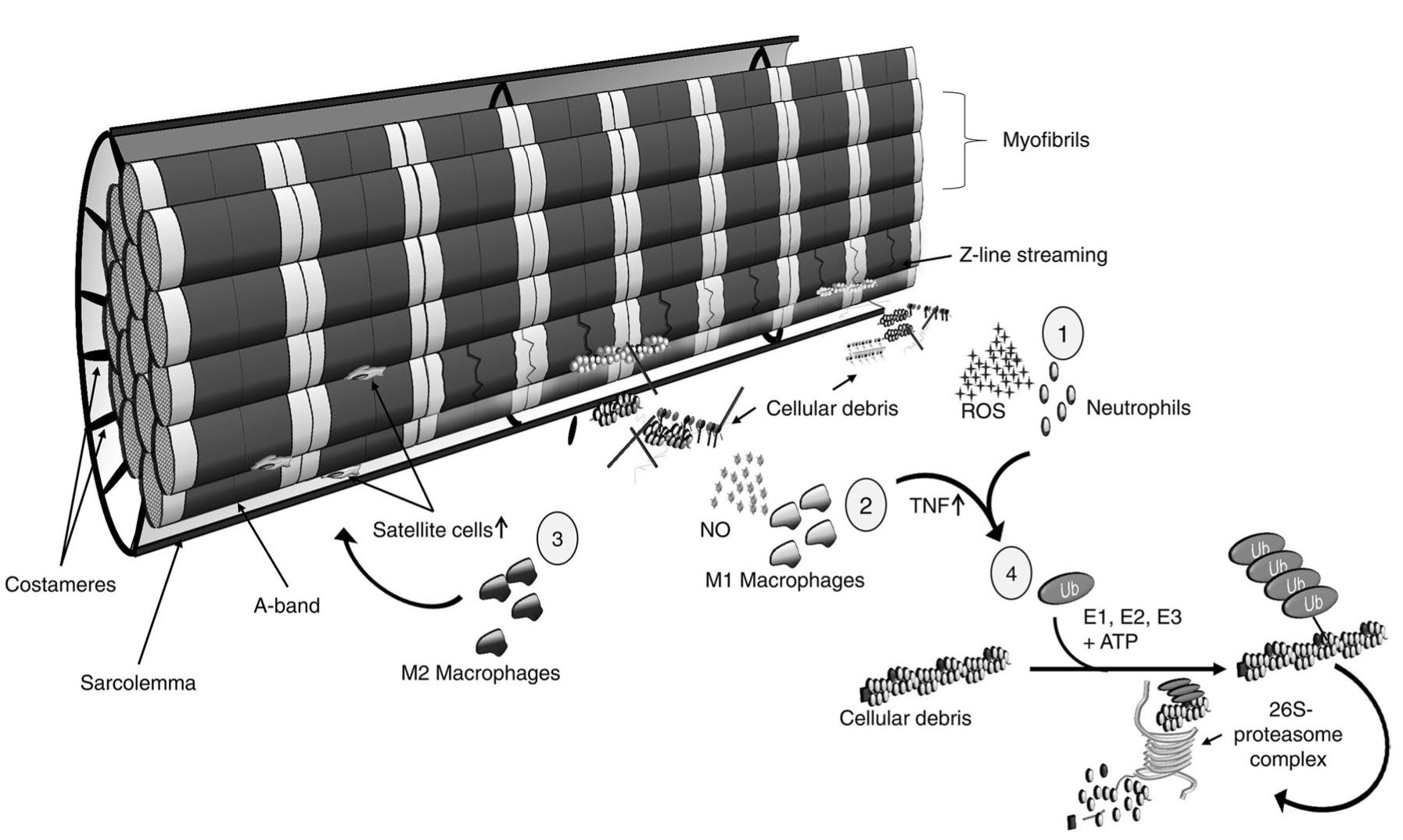
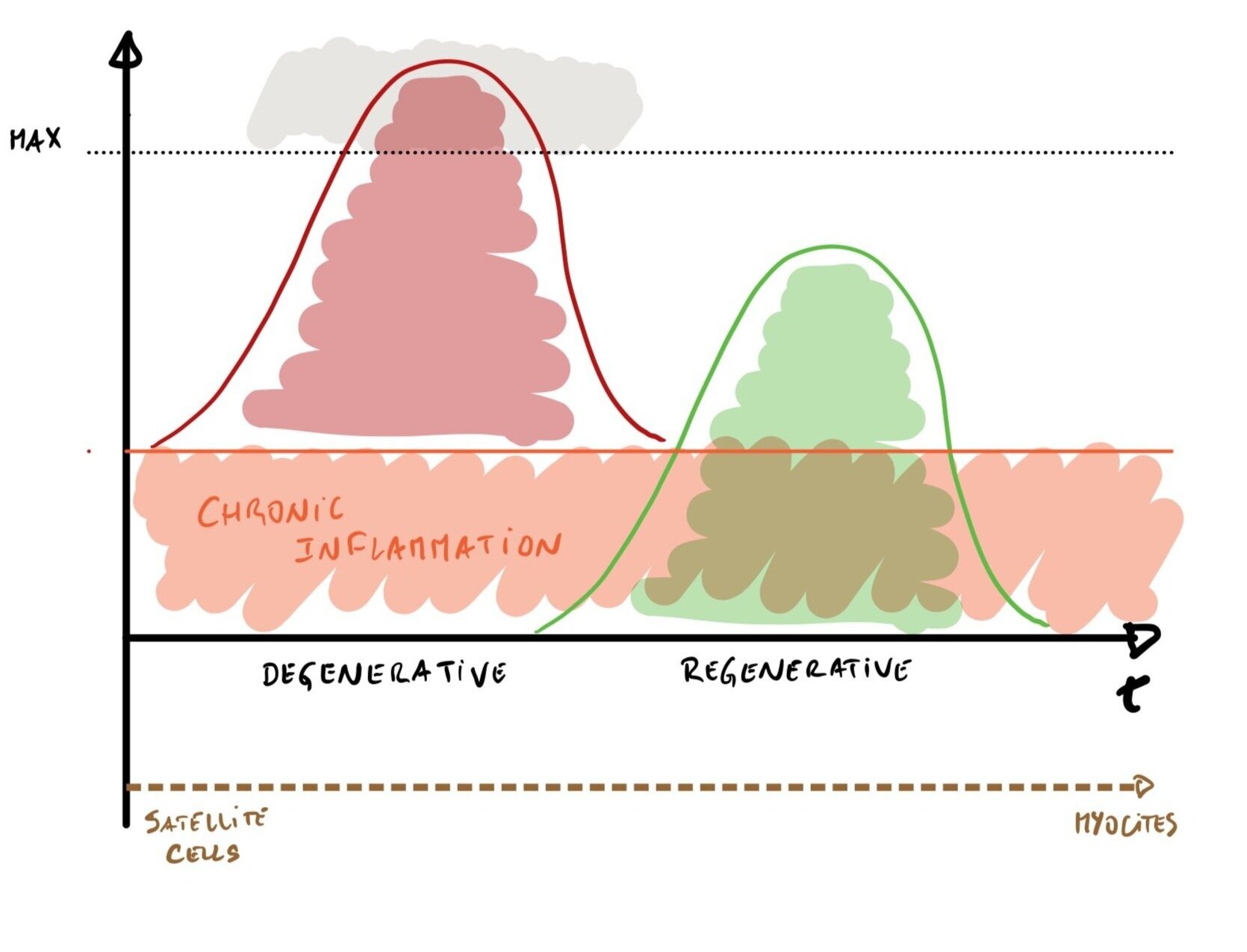
Quando treinamos, estamos a (querer) causar dano nas fibras musculares; só assim conseguimos desencadear os fenómenos de adaptação e regeneração do tecido. É o primeiro passo de uma série de acontecimentos que irá resultar na criação de novas células musculares a partir de células estaminais específicas, as células satélite.
A primeira fase é a pró-inflamatória ou degenerativa. É catalizada pelo dano infligido às células musculares e pela consequente libertação de mediadores inflamatórios, como espécies reactivas de oxigénio (ROS), IL6 e TNFa, e mobilização de neutrófilos e macrófagos M1, as principais células intervenientes neste passo. Em conjunto, trabalham para destruir os escombros e os detritos da célula danificada, assegurando que o terreno está pronto para ser restaurado e fortalecido.
Quanto maior o dano, maior a magnitude do processo pró-inflamatório desencadeado e, por essa razão, maior a intensidade do processo de destruição e limpeza.
Quando a limpeza é concluída, o cenário muda significativamente: a pró-inflamação transforma-se em anti-inflamação dando origem à segunda fase, a de regeneração. Os mediadores do processo mudam (há um aumento da quantidade de IL10, um citoquina anti-inflamatória), há libertação de factores de crescimento (HGH, TGF B1 e IGF-1) e os macrófagos passam a M2, dando ordem às células satélite (que entretanto aumentaram em número por acção dos M1) para se transformarem em células musculares.
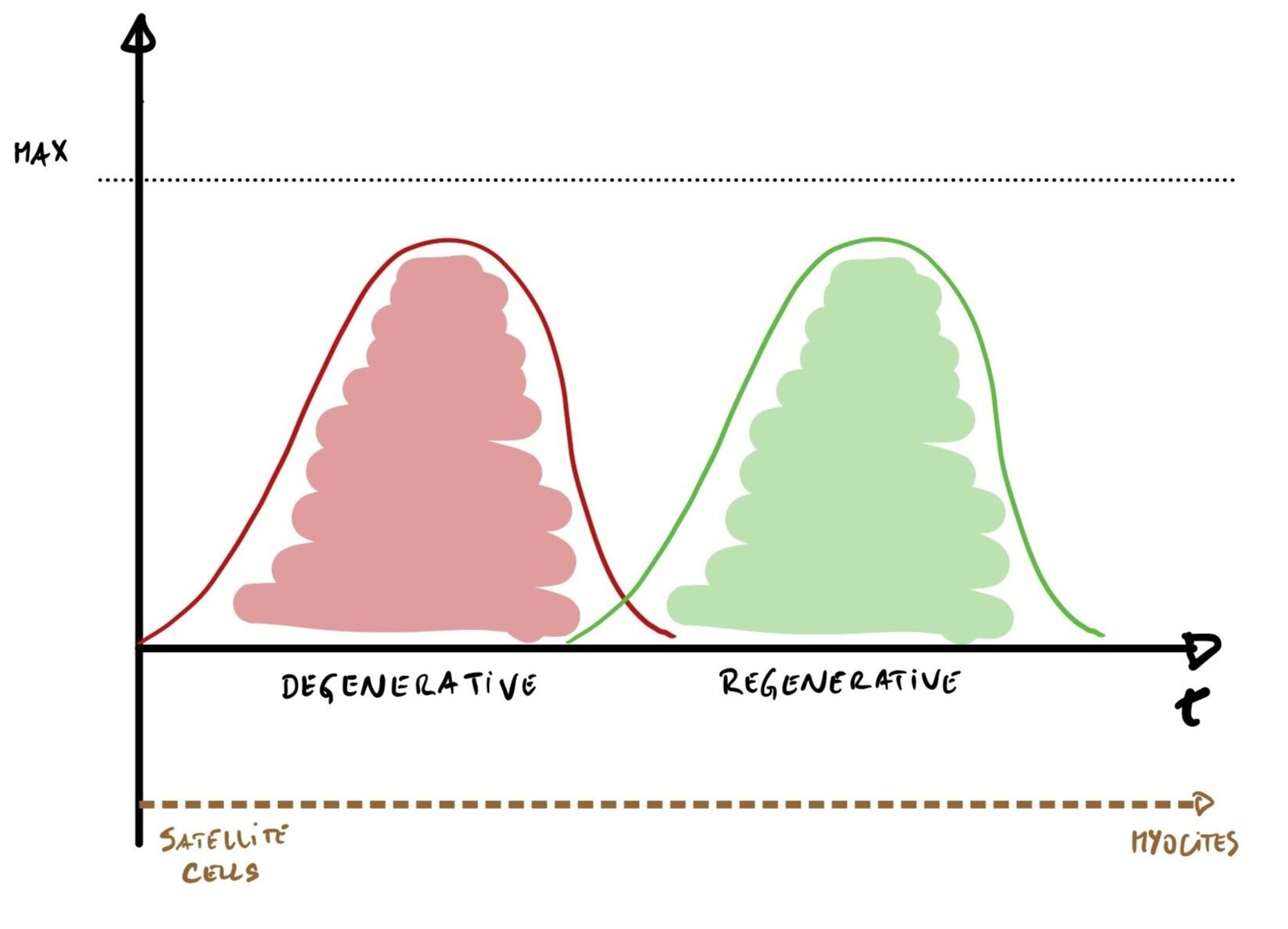
É este equilíbrio entre aumento e diminuição da inflamação que evoluímos. A palavra chave é mesmo essa: equilíbrio.
O sucesso deste processo depende da existência de um pico inflamatório, causado pelo aumento dos mediadores inflamatórios que sinalize o início da primeira fase, que dê origem a um pico anti-inflamatório de magnitude adequada de modo a fazer face ao sinal inflamatório emitido. Só assim as células satélite se irão transformar em células musculares, regenerando e fortalecendo o músculo.
Qualquer distúrbio na magnitude de ambos os picos prejudica todo o processo:
Se o pico inflamatório for demasiado pequeno, pode não ser suficiente para desencadear o ciclo (se o esforço e o stress exercido for pequeno, provavelmente não vai levar a ganhos reais)
Se não houver capacidade anti-inflamatória, não será possível reparar o dano
Se o pico inflamatório for muito grande, é provável que o dano causado seja demasiado para poder ser reparado, requerendo um trabalho longo e eventualmente imperfeito (o que cumulativamente pode levar ao overtraining syndrome).
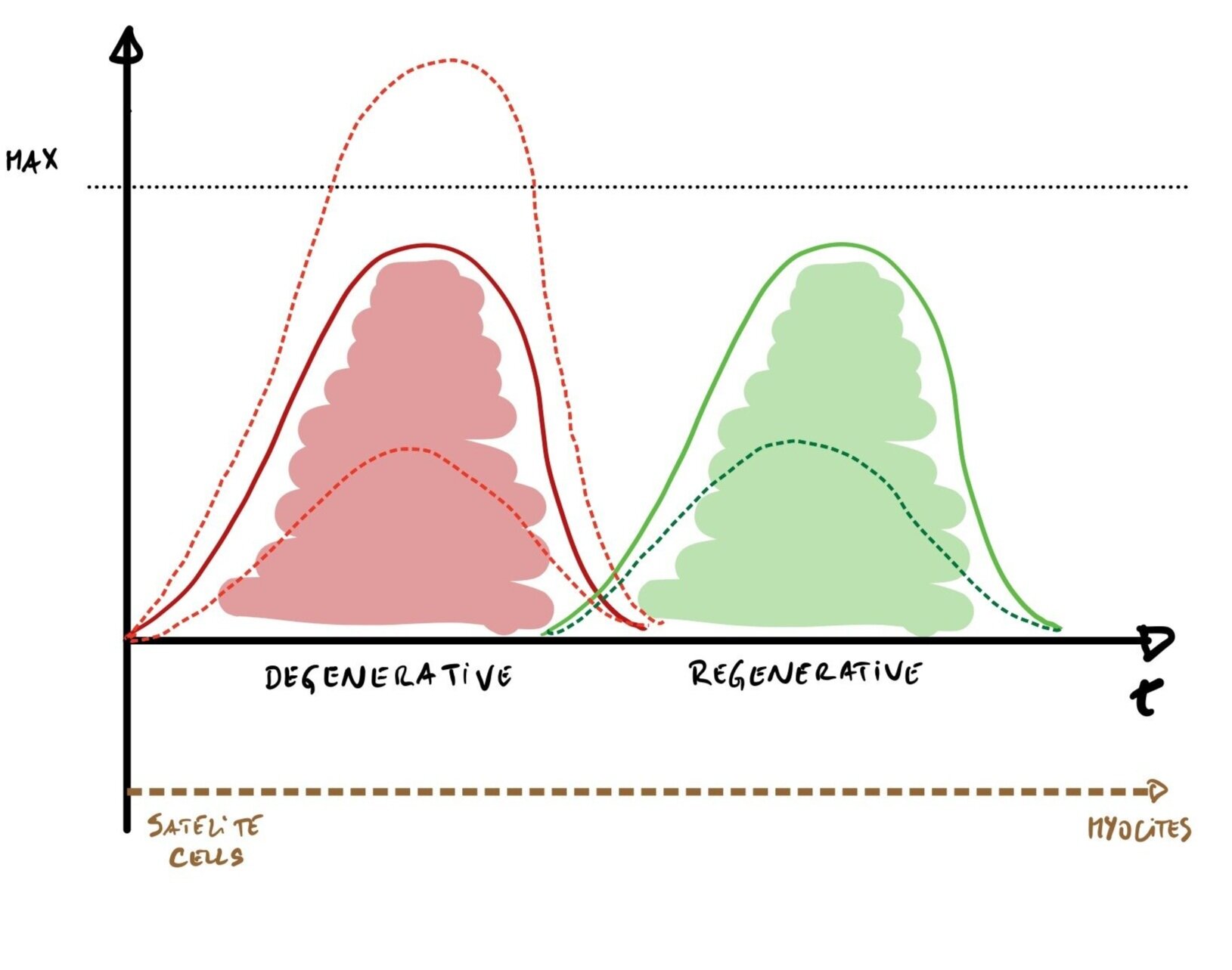
Há ainda outra forma de desequilíbrio: a existência de um estado crónico de inflamação.
Neste estado, há informação a circular constantemente a sinalizar a libertação de mediadores pró-inflamatórios, criando um estado de inflamação crónica de baixo grau. Este estado é conhecido por estar associado a diversos processos de doença crónica, desde a diabetes, depressão, doenças cardiovasculares e até oncológicas.
No contexto de performance, o seu impacto está longe de ser positivo:
Como é que o impacto pode ser tão abrangente?
Porque estes quadros inflamatórios crónicos não só dificultam a adaptação das estruturas ao esforço físico como aumentam o desgaste e o dano acumulado.
Para que o processo de recuperação e adaptação seja desencadeado, é necessário que haja um determinado aumento dos mediadores pró-inflamatórios, um determinado delta, para que todo o processo decorra. Sem esse aumento, não se vai dar início ao ciclo de recuperação.
Contudo, quando a quantidade de mediadores inflamatórios que existem em circulação já está cronicamente aumentada, a elevação necessária pós-treino parece estar comprometida. Isto foi demonstrado para as citocinas mais cruciais neste processo, como a IL6 e também o TNFa.
Se não se consegue ter esse pico inflamatório pós-esforço, quando ele é realmente obrigatório, todo o processo fica comprometido, levando às conclusões que parecem agora óbvias, como é dito neste artigo de revisão de 2016:
"As dificuldades de recuperação pós-exercício podem dever-se apenas à dificuldade que é aumentar as citocinas pró-inflamatórias num indivíduo já cronicamente inflamado "
Dito por outras palavras, o aumento destas citocinas, independentemente da razão ou origem no nosso organismo, irá dificultar a recuperação e, pela mesma razão, a performance. O que nos traz de volta às intolerâncias alimentares e à razão pela qual podem ter sido uma peça chave para o título mundial de Lucy Charles-Barclay.
Cada vez que Lucy comia alimentos aos quais era intolerante, estava a dar origem ao aumento dos mesmos mediadores inflamatórios que precisa de ter extremamente controlados para poder treinar, recuperar e competir ao mais alto nível. Se ingerir esse alimento 3 vezes por dia, será esse o número de picos de libertação desses mensageiros. Se aliarmos esse dado ao plano de treinos altamente exigente que segue, com 2 a 3 treinos diários (que também criam picos), a magnitude do status inflamatório cresce significativamente.
A consequência, prevejo eu com base em tudo o que descrevi, terá sido um aumento desnecessário desses mensageiros ao longo do tempo, criando um estado inflamatório cronicamente mais elevado do que seria desejável, com potencial impacto negativo na sua performance.
Pela mesma razão, quando retirou do plano as suas intolerâncias alimentares, a agora campeã do mundo terá necessariamente atingido um maior equilíbrio imunitário com potencial para melhor a sua performance, mesmo que tenho sido 1 a 2%. Ao longo de 4 horas de prova, são minutos cruciais ganhos.
A influência da alimentação na performance, desportiva ou não, vai muito para lá da quantidade de macro ou micronutrientes.
É muito mais do que combustível. O efeito inflamatório da dieta é uma factor provavelmente mais importante e com maior influencia na capacidade e probabilidade de atingir os melhores resultados, seja ser campeão mundial ou superar um dia de reuniões exigentes. Não se trata só de "comer bem" ou "ter uma dieta limpa" mas sim de saber o que é o melhor para cada sistema, cada atleta, cada indivíduo.
Só assim conseguimos atingir o nosso melhor potencial. Não é isso que todos procuramos?
Duas notas finais:
Neste artigo simplifiquei significativamente a fisiologia e a bioquímica com o objectivo de torná-las de melhor compreensão. Essa simplificação não alterou no entanto a veracidade dos argumentos descritos. Se quiser mergulhar nos detalhes, convido-o a ler os artigos que referencio ao longo do texto, são fascinantes).
A relação entre sensibilidades alimentares e desportos, em particular de endurance, é complexa, em particular pelo impacto na saúde gastrointestinal que provas de longa duração tem. Estão descritos casos de aumento de permeabilidade intestinal em consequência do esforço físico, aumentando por essa razão a reacção inflamatória intestinal e não por acção primária causada pela alimentação. Apesar de a causa ser diferente, e daí o tratamento desses quadros seja diferente, mesmo nessas circunstâncias os alimentos despoletam reacções imunitárias podendo agravar o quadro. Por essa razão, e ainda que de forma transitória, há provavelmente benefícios claros em estudar as reacções alimentares e retirar esses alimentos do plano alimentar).