Mais um prego no caixão da ausência de evidência do Protocolo Coimbra
Desde que prescrevo o Protocolo Coimbra me perguntam qual a base científica para a sua prescrição. É uma questão naturalmente justa, sem dúvida. Seja pela curiosidade de quem quer saber como funciona a vitamina D e porque é necessária a toma de altas doses, seja porque os seus médicos levantam essa dúvida - de uma forma mais ou menos incisiva ou agressiva -, a verdade é que me vejo confrontado com alguma variação desta questão.
Na minha resposta acabo por explicar a fisiologia da vitamina D, a maneira como funciona no núcleo das células, as particularidades genéticas envolvidas no seu metabolismo e o racional para serem necessárias doses significativamente mais altas do que o recomendado. Tento fornecer tanta informação e dados quanto seja necessário para responder às questões que me são colocadas e garantir que a pessoa que decidiu sair do caminho terapêutico mais óbvio e procurar vias diferentes sinta que tomou a decisão certa e que tem o suporte que merece.
O argumento de que o Protocolo Coimbra não tem evidência para o seu uso é falso. Neste texto explico detalhadamente a evidência que está por trás do uso de altas doses de vitamina D.
"Não é suficiente", dizem os críticos, "não existe nenhum artigo peer-review publicado numa revista importante que suporte a sua prescrição". De facto verdade, até este ano.
Em Abril de 2021 foi publicado por colegas alemães, liderados por Dirk Kemke e Beatrix Schweiger, um artigo entitulado "Vitamin D Resistance as a Possible Cause of Autoimmune Diseases: A Hypothesis Confirmed by a Therapeutic High-Dose Vitamin D Protocol".
É um marco muito importante porque, pela primeira vez, foi publicado um artigo numa revista de renome, a Frontiers in Immunology, revisto por líderes mundiais no campo de investigação da vitamina D, suportando o uso do Protocolo Coimbra em doenças autoimunes.
É um artigo denso e fascinante, expondo de forma estruturada e clara a evidência existente. Quem gostar de mergulhar nos detalhes e nuances da ciência, aconselho vivamente a sua leitura.
Estas são as 3 ideias principais do artigo:
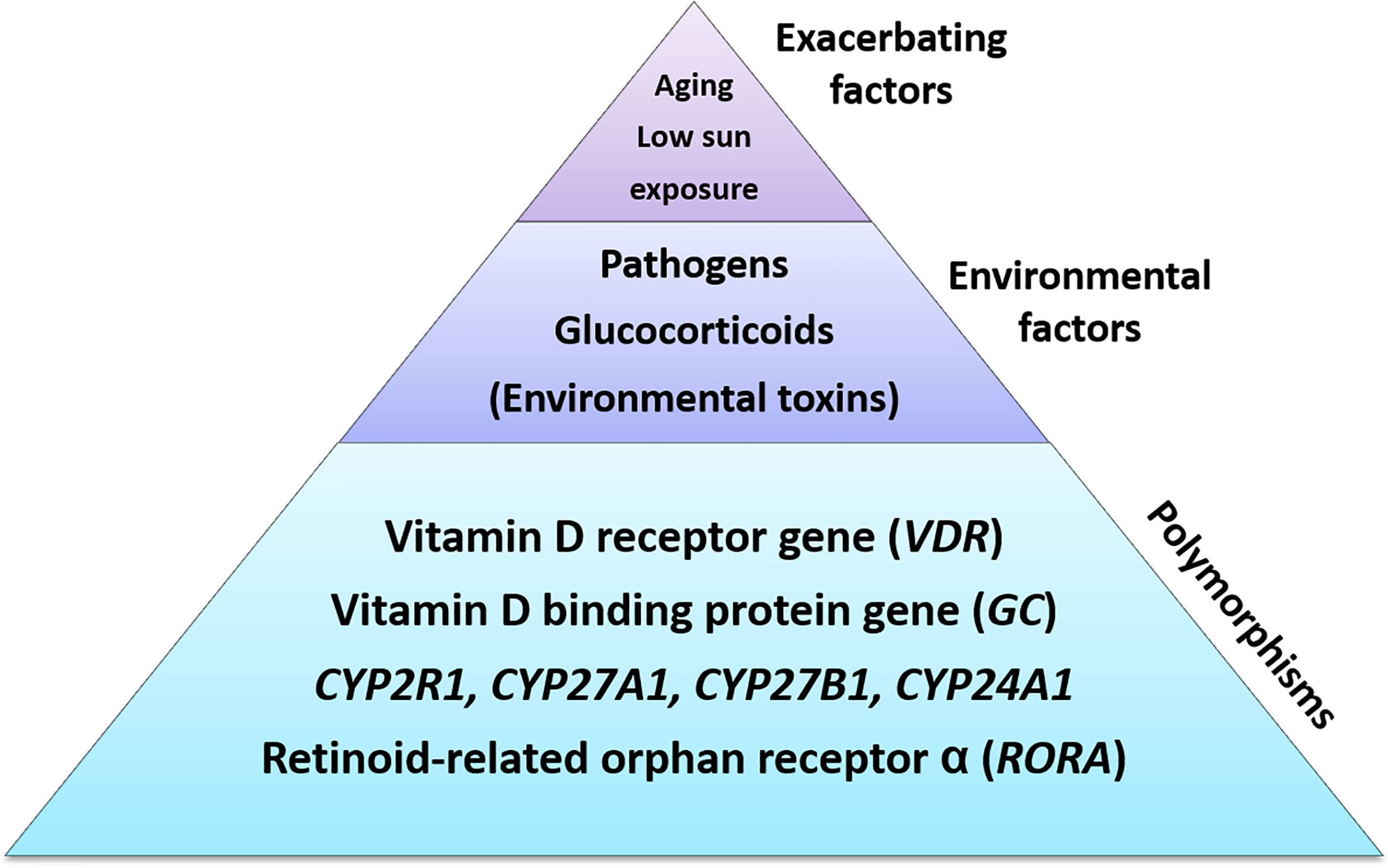
Polimorfismos nos genes do sistema da vitamina D podem criar susceptibilidade individual para o desenvolvimento de baixa resposta à vitamina D, sendo a resistência adquirida à vitamina D uma forma extrema, exacerbada por outros factores causadores de bloqueios no receptor da vitamina D.
Este ponto e toda a justificação científica apresentada é particularmente fascinante porque esclarece a porquê da resposta dos nossos doentes à pergunta "porque acha que a doença apareceu ou agravou".
Invariavelmente, a resposta que nos dão é "stress".
Mais de 95% dos nossos doentes diz-nos que a sua doença autoimune foi despoletada ou agravada após um período mais ou menos intenso de stress, em particularmente stress físico ou emocional. Os exemplos mais comuns são fracturas relacionais ou condições laborais stressantes e difíceis, ainda que haja exemplos que momentos supostamente felizes como gatilho para o agravamento, como preparação para o casamento ou nascimento do primeiro filho.
Já tinham sido publicadas diferentes hipóteses possíveis para o porquê dessa relação, variando desde a alteração da regulação das células Treg (a que eu chamo "maestros da imunidade") ou ao impacto de níveis aumentados de forma crónica do cortisol, a hormona do stress, embora, a meu ver, sem serem capazes de esclarecer de forma pormenorizada essa relação, algo que este artigo conseguiu fazer.
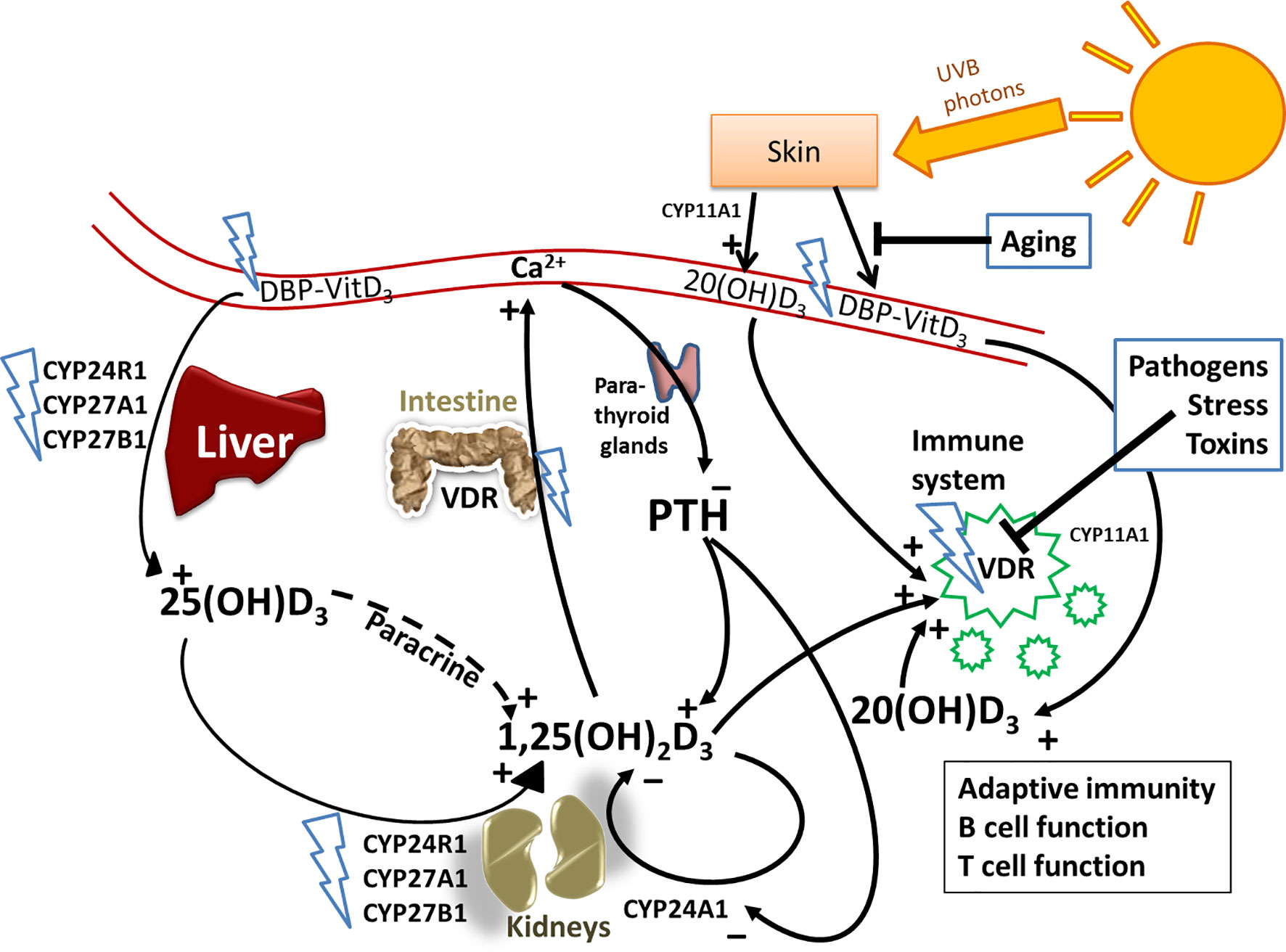
Tentando simplificar a ciência descrita, o aumento de glucocorticoides (cortisol, cortisona ou derivados) inibe o receptor da vitamina D, VDR. Essa inibição impede que a vitamina D se ligue ao receptor e, dessa forma, impede o efeito positivo desta vitamina na otimização da função imunitária. Dito de outra forma, a existência de níveis aumentados de cortisol e companhia em resposta a stress (qualquer que seja) criam um bloqueio do receptor da vitamina D, criando as condições para o aumento da intensidade das respostas autoimunes.
É muito provável que seja esta a razão pela qual o stress, em particular o emocional, é a principal barreira que bloqueia o efeito positivo do Protocolo Coimbra.
Retirada do artigo
Mas este impacto pode, e talvez deva mesmo, ser extrapolado para qualquer outro factor que influencie a negativamente o VDR, nomeadamente infecções, suportando uma vez mais a observação da existência de um agravamento clínico durante infecções víricas ou bacterianas.
2. “Nível de hormona paratiroide no sangue mantêm-se como a informação chave para a determinação da dose de vitamina D nas doenças autoimunes enquanto não existir outra forma de determinar a resposta individual à vitamina D”
Não podia ser dito de melhor forma: até que exista melhor forma de medir o efeito biológico real da vitamina D, somos obrigados a recorrer à medição da hormona paratiroidea (PTH).
Os níveis de PTH variam de forma inversa em função do efeito biológico da vitamina D, não da sua concentração sanguínea. Aliás, um estado de hiperparatiroidismo secundário é uma indicação analítica de provável resistência genética à vitamina D, em particular quando os níveis de vitamina D no sangue estão "normais" (isto é, dentro dos níveis de referência).
Por esta razão, quando o efeito biológico da vitamina D aumenta, a PTH diminui. Tal e qual como uma balança, quando um dos pratos sobe, o outro desce. Assim, para atingir o alvo terapêutico do Protocolo Coimbra e conseguir o efeito biológico máximo da vitamina D, aumentamos a sua dosagem até a PTH estar baixa - preferencialmente abaixo do intervalo de referência.
Como costumo dizer aos nossos doentes, não há nada mágica na PTH e nos seus valores estarem baixos. Isso apenas significa que atingimos o que queremos: o efeito máximo da vitamina D.
3. “Tendo por base estes dados, a terapia com altas doses de vitamina D deve ser incluída nas medidas terapêuticas para todas as doenças autoimunes numa base individual apenas”
Se somos todos diferentes, é absolutamente lógico que precisemos de quantidades diferentes dos mesmos compostos. Parece-me algo óbvio. A mesma dose de qualquer composto fará efeito nalgumas pessoas enquanto que noutras não. O tratamento com insulina será sempre o exemplo mais clássico - e convencional - da necessidade de personalizar os tratamentos.
Imagem retirada do artigo
Não é possível generalizar uma dose de vitamina D: a mesma dose pode extremamente tóxica ou absolutamente ineficaz quando tomada por pessoas diferentes.
As características genéticas, a existência de factores que possam influenciar o metabolismo desta vitamina influenciam o processo e definem quais os passos necessários para atingir o sucesso terapêutico. Não se trata apenas de prescrever suplementos em determinadas doses, ajustadas a resultados analíticos. Trata-se também de eliminar razões que possam influenciar negativamente o curso do tratamento, em particular o stress.
A experiência acumulada ao longo destes anos ensinou-me que a parte "fácil" de prescrever o Protocolo Coimbra é a parte técnica: gerir a vitamina D, o seu efeito positivo, os seus riscos e assegurar que os doentes estão seguros.
Mais difícil mas mais desafiante é apoiar a pessoa que toma a decisão corajosa de sair do caminho mais fácil e óbvio e procurar melhores soluções para a sua doença, reduzindo as dúvidas e inseguranças inerentes à decisão.
Prevejo que com o passar do tempo, com cada vez mais milhares de pessoas a serem ajudadas pela vitamina D de uma forma ou outra, o reconhecimento científico será cada vez maior do potencial que a vitamina D tem nas diferentes doenças autoimunes.
Esse reconhecimento aumentará a segurança e certeza de quem inicia o Protocolo Coimbra, deixando de se sentir "aves raras" ou hereges por terem decidido por um caminho fora do normal, diminuindo o stress associado à escolha do tratamento.
Este artigo é um passo muito importante nessa direcção.