Doenças Inflamatórias do Intestino: há que combater a inflamação crónica
A doença inflamatória intestinal é a designação que se dá a um conjunto de doenças relacionadas com o trato digestivo: Doença de Crohn, Colite Ulcerosa e Colite Microscópica.
Mais de 20 mil portugueses são afectados por estas patologias, cujo dia internacional se comemora a 19 de Maio e cujas campanhas de sensibilização já são comuns todos os anos.
Não sendo patologias de elevada mortalidade, são motivo de perda de qualidade de vida.
A inflamação crónica é a característica comum à doença de Crohn e à colite ulcerosa sendo que, a doença de Crohn, pode afectar todo o sistema digestivo e a colite ulcerosa apresenta-se normalmente no cólon e reto. No que respeita à extensão da doença, na doença de Crohn é maior, notando-se que a própria parede intestinal é mais extensamente afectada, do que na colite ulcerosa. Em ambos os casos, os efeitos podem acabar por se notar em todo o corpo (olhos, articulações, pele, entre outros). São doenças consideradas imunitárias, já que o sistema imunitário reage contra o próprio corpo.
A patofiosiologia da colite ulcerosa e da doença de Crohn são distintas, apresentando no entanto algumas semelhanças.
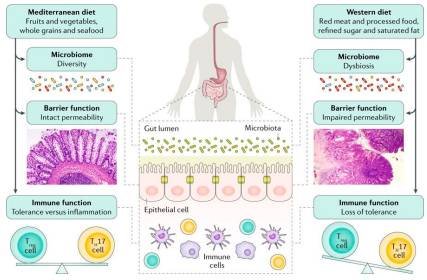
Em ambas, a mudança na diversidade bacteriana da flora intestinal, alteração da barreira epitelial e da barreira mucosa através da disrupção das chamadas “tight junctions” são o ponto de partida para a activação do sistema imunitário. Esta alteração da permeabilidade intestinal, leva a que o sistema imunitário entre em contacto com bactérias da flora intestinal levando à produção de mediadores inflamatórios que vão ter inúmeros efeitos (TNF-α, IL-5, IL-6, e IL-13 no caso da colite e TNF-α, IL-6, and IL-23 no caso da doença de Crohn). As vias que se activam depois disto são distintas e podemos discuti-las numa outra oportunidade.
Os sintomas digestivos acabam por ser parecidos: cólicas, movimentos intestinais frequentes (normalmente no sentido de diarreia), muita formação de gás. A perda de peso, febre, suores nocturnos, cansaço, anemia,... são sintomas também comuns, com o passar do tempo. Estes sintomas podem todos desaparecer e voltar sem razão aparente (períodos de remissão e de crise). A inflamação que está por trás destes sintomas é que é crónica e deve ser de alguma forma controlada.
Aqui é que está o centro da questão. A inflamação.
Este nosso aliado, que deixa de o ser quando passa a ser crónico. E a modulação imunitária.
O método de diagnóstico destas doenças é através do relato do paciente (sinais e sintomas), avaliação clínica e exames como análises sanguíneas (detectam por exemplo a existência da inflamação), avaliação às fezes (calprotectina, lactoferrina, entre outros marcadores), endoscopia ou ileocolonoscopia, exames por tomografia computorizada, ressonância magnética e videoenteroscopia por cápsula. Em casos mais graves, pode ser preciso operar a zona afectada. Normalmente actua-se dando algumas indicações alimentares e/ou sugerindo medicação (anti-inflamatórios que atuam no intestino - aminosalicilatos), corticóides, antibióticos, fármacos imunossupressores ou medicamentos biológicos).
Há pacientes que simplesmente tomam sempre a medicação e dão-se bem com isso (cada um escolhe o seu caminho). Mas, há medicamentos que não se podem tomar continuamente e há pacientes que, de qualquer forma, preferem outras opções. Para quem talvez queira outro caminho, há outras hipóteses.
Imaginemos como analogia, que no nosso carro se acende a luz do óleo do motor. Nós sabemos bem o que esta luz significa e portanto, idealmente enchemos de novo o depósito do óleo. Mas, se só quisessemos livrar-nos do sintoma (luz do óleo do motor que está acesa), poderíamos encher o depósito com água ou, em último caso, até partir o mostrador do sinal. O sintoma desaparece (luz acesa), mas o problema continua a estar no carro.
O que fazemos ao tomar medicações durante anos sem fazer mais nada em termos de controlo da inflamação e imunidade, é como colocar água no motor ou partir o mostrador.
Podemos até ter análises a mostrar valores inflamatórios mais baixos, ou uma imunidade mais controlada, mas, a causa da inflamação continua a não ser tratada. Ela está simplesmente mais baixa porque uma medicação está a forçar isso.
Não estou com isto a dizer que conhecemos a cura da doença, até porque as suas causas não são ainda claras. Há situações em que os medicamentos são necessários, nem que seja temporariamente; ou outras em que o quadro clínico já evoluiu muito negativamente (obstrução intestinal, fístulas,...), sendo precisas abordagens mais agressivas como até a cirurgia. Mas, podemos de alguma forma (e já o fazemos) tentar combater de outra forma a inflamação que está num estado crónico, permitir melhor modulação imunitária, dando ferramentas ao corpo para o fazer (colocando o óleo certo no motor).
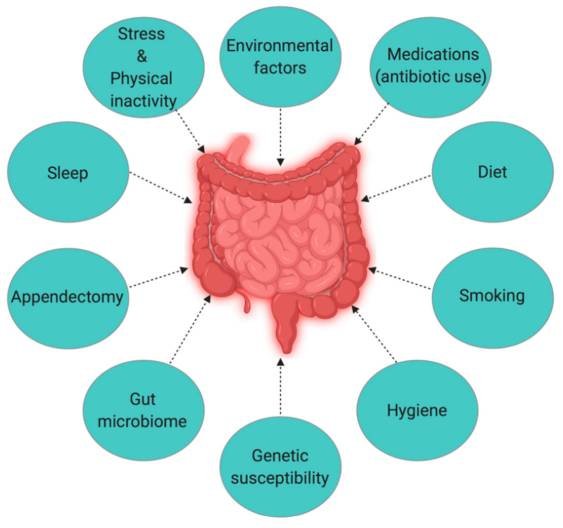
Fatores ambientais envolvidos na Doença Inflamatória do Intestino.
Voltemos por uns instantes, às causas que são ainda desconhecidas, mas das quais temos algumas pistas. Sabe-se que há uma componente genética associada (se tiver um familiar com a doença, a sua probabilidade de ter é maior), mas também que são os factores ambientais que activam essa susceptibilidade. Factores como hábitos de sono, stress e inactividade física, flora intestinal (microbioma), hábitos tabágicos, maus hábitos alimentares (principalmente muito industrializados), uso de medicamentos (uso de antibióticos por exemplo).
Ora se se sabemos que estes são os factores que possivelmente levam ao aparecimento destas condições, é pois também aqui, que devemos actuar no tratamento. As sugestões de actuação nos casos de doença inflamatória intestinal são, por isso, bastante abrangentes.
Se quer tratar de si, tem de olhar para si como um todo que merece um novo plano de acção, porque o que fez até agora não resultou. A nutrição é uma parte integrante mas não só:
Mantenha-se activo. O sedentarismo aumenta o risco de uma série de problemas e também de doença inflamatória do intestino. Outra vez isto do exercício? Pois, já pensou se se se fala tanto nisso é porque é mesmo preciso mexer-se! A actividade física está associada directamente à diminuição de marcadores inflamatórios.
Diminua a ingestão de açúcar simples e tenha atenção às combinações alimentares do seu dia-a-dia. Sim, se passar o dia a fazer snacks e/ou a entrar em hiperglicemia está a ter um efeito pró-inflamatório (favorecedor da inflamação). De cada vez que come está a enviar uma mensagem ao seu corpo. Que tipo de mensagem quer mesmo enviar?
Controle o stress, ou pelo menos da forma como interpreta as situações stressantes na sua vida. Não é realista pedir-lhe que elimine o stress do seu dia-a-dia, mas é realista (e necessário), que encare o stress de uma outra forma, que encontre as suas estratégias para lidar com ele e que sim, se calhar se livre de uma ou outra situação ou pessoa tóxica da sua vida. O seu intestino agradece.
Melhore o estado nutricional. Tem uma vitamina D normal (agora até é comum medir), mas pode e deve melhorar o seu valor. Pode ser uma das pessoas com maiores necessidades. Tem um valor baixo? Está à espera de quê para tratar disso?
Melhore ainda mais o estado nutricional.Outras vitaminas e minerais devem ser colocadas em cima da mesa: magnésio, zinco, ferro, vitamina B6, vitamina C, vitamina E. Fitoquímicos e outros antioxidantes.
Durma bem: mais de 6 horas de sono, mas menos de 9 parecem ser o ideal. Tente ter um fim de dia calmo, para que a sua melatonina suba e consiga dormir bem.
Evite o uso de antibióticos podem levar a alterações da flora intestinal que potenciam o risco de doença intestinal. Assim, tome só mesmo em casos estritamente necessários.
Use apoios extra como com curcuma, ómega 3 , resveratrol, gengibre (efeito muito interessante na flora intestinal e de anti-inflamação), probióticos,... dependendo dos casos podemos experimentar diversos elementos.
Alimente-se privilegiando fontes antioxidantes e potenciadoras da imunidade. Poderia estar a falar de uma alimentação mediterrânica, cetogénica, baixa em FODMAPS, ou de qualquer outro tipo de abordagem. O importante é que se consigam os nutrientes necessários, focando primeiramente no que parece estar em falta, em gorduras de qualidade, proteínas suficientes mas não em demasia. A tolerância de cada paciente é que ditará o caminho.
O acompanhamento nutricional e/ou médico tem de ser verdadeiramente personalizado, pois cada paciente é efetivamente único.
Se quiser dar início à sua jornada de saúde connosco, pode contactar-nos:
E. info@cristinasales.pt
T. (+351) 911 082 191